A medical claim is a detailed invoice that a health care
provider sends to the health insurer, exactly showing the services that have
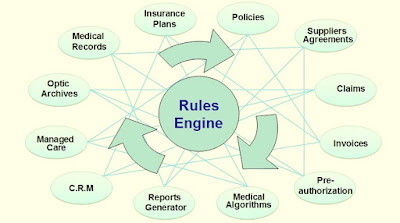
been rendered by the providers to the patient. Medical claims management involves
multiple administrative and customer service layers that include review,
investigation, adjustment, remittance or denial of a claim. Improved focus on
quality healthcare services and adoption of cloud technology related services are
contributing to the growth of the
medical
claims management solutions market. Medical claims management solutions generally aim at attaining
complete automation of processing of claims, faster access to customer
information without negotiating on the security of private medical information.
However, insurance claim payers and providers need to be convinced about the
need for these solutions and also the benefits of investing in them despite
their sizeable cost. Automation helps in reducing costs associated with
processing of claims, utilizing a single platform for all data sources,
workflows for routing claims for review and approval processes, increasing the uniformity
of payments, and timely payment of claims. According to the National Health
Insurer Report Card published in 2011 by American Medical Association (AMA), around $17 billion a
year (on an average) could be saved by eliminating errors in claims. Automation
reduces the paper storage and document retrieval costs while complying with regulatory
standards such as Health Insurance Portability and Accountability Act (HIPAA). Health
insurance payers invest in their claims management systems to gain
interoperability and faster release of new insurance claims, in addition to,
improving efficiency of claims processing.
The increasing investment in the healthcare infrastructure and services in Asia-Pacific offers huge market potential for the players to grow in medical claims management solutions market. Countries such as India and China are the two rapidly growing economies in the Asia-Pacific region, followed by South Korea. The government in these countries are putting in several efforts to provide better healthcare services and improved healthcare infrastructure. Healthcare IT related services bridge the gap between healthcare entities by lowering down the manual errors and also reducing healthcare expenditure. However, the healthcare IT industry in India is at its nascent stage. Thus, heavy inflow of investments by various government agencies to improve healthcare IT infrastructure in emerging markets is expected to create opportunities for healthcare claims management solutions providers.
Explore Report Sample at: https://www.psmarketresearch.com/market-analysis/medical-claims-management-solutions-market/report-sample
The major players in the medical claims management solutions market include IBM Corporation, Cerner Corporation, Oracle Corporation, Avaya Inc., Genpact Limited, Cognizant Technology Solutions Corporation, Accenture PLC, Allscripts Healthcare Solutions, Inc., Athenahealth Inc., Aspect Software Inc., and Infor Inc.
No comments:
Post a Comment